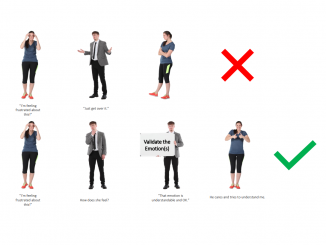
One of the common phenomenons I see in relationship counselling is the link between stress, emotionality, and safety in the home.
In short, stressed people are generally more emotional (Fight or Flight response triggered for example), and people in an emotional state are probably more likely to be causing damage to their relationship, naturally, damage to the relationship can mean decreased safety at home.
That’s a pretty stressful place to be…and a typical cycle or bind that people can find themselves in.
That stress can also affect the way our brain functions, both directly, by way of the release of the stress-response hormone, Cortisol, but also indirectly through our gut health.
Most agree, having a healthy tummy is a key ingredient in better emotional wellness, and a new study out of the UK has again backed this opinion.
Researchers from the UK’s University Psychiatric Clinics Basel have shown that probiotics can support the effect of antidepressants and help to alleviate depression.
Previous studies involving people with depression show an above-average prevalence of intestinal and digestive problems.
In the new study, the researchers gave participants (inpatients at the University Psychiatric Clinics Basel) a probiotic or a placebo for 31 days, in addition to antidepressants.
Neither the participants nor the study staff knew which preparation they were taking throughout the study.
The researchers carried out a series of tests on the participants immediately before treatment, at the end of the 31 days, and again four weeks later.
Subsequent analysis showed that although depressive symptoms decreased in all participants thanks to the general antidepressant treatment, there was a greater improvement in the subjects in the probiotic group than in the placebo group.
In addition, the composition of their intestinal flora changed, at least temporarily: in the probiotic group, an analysis of stool samples revealed an increase in lactic acid bacteria at the end of treatment, an effect that was accompanied by a reduction in depressive symptoms.
However, the level of these health-promoting gut bacteria decreased again over the following four weeks.
“It may be that four weeks of treatment is not long enough and that it takes longer for the new composition of the intestinal flora to stabilize,” – Anna-Chiara Schaub, one of the lead authors of the study.
Another interesting effect of taking probiotics was seen in relation to brain activity when viewing neutral or fearful faces.
The researchers investigated this effect using functional magnetic resonance imaging (fMRI).
In patients with depression, certain brain regions for emotional processing behave differently than in individuals with good mental health.
After four weeks of probiotics, this brain activity normalized in the probiotic group but not in the placebo group.
“With additional knowledge of the specific effect of certain bacteria, it may be possible to optimize the selection of bacteria and to use the best mix in order to support treatment for depression,” says the researcher, although she is keen to emphasize that probiotics are not suitable as a sole treatment for depression.